Abstract
Background: For some rare cancers, better outcomes have been reported for patient (pts) treated at high volume or specialty centers compared to pts who did not receive such care. Greater availability of interventional clinical trials may be one of the drivers of better outcomes in specialty centers. However, not all pts referred to specialty centers are eligible or willing to participate in trials, and it is not known how outcomes compare for pts treated at specialty centers on clinical trials versus standard of care. In this study, we compared the outcomes of higher-risk MDS pts treated in and out of clinical trials at MDS specialty centers.
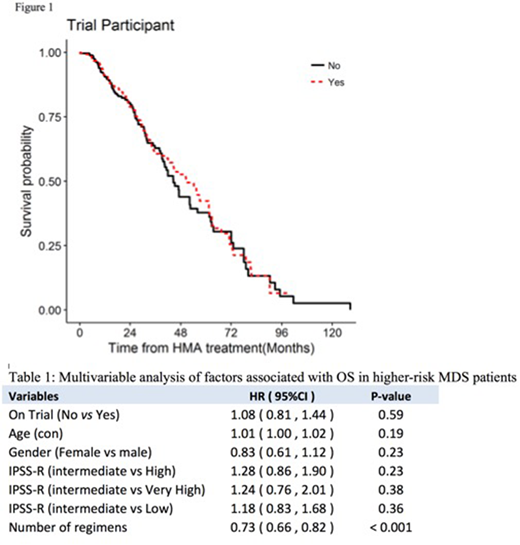
Methods: Pts treated at MDS Clinical Research Consortium institutions (Moffitt Cancer Center, Cleveland Clinic, MD Anderson Cancer Center, Cornell University, Dana-Farber Cancer Institute, and Johns Hopkins) from 2006-2016 were included. Pts were diagnosed with MDS according to 2008 WHO criteria and identified as having "higher-risk" disease based on the revised IPSS (IPSS-R) criteria that included Intermediate, High and Very high risk categories. All pts treated outside clinical trials received hypomethylating agents (HMAs), either azacitidine (AZA) or decitabine (DAC). Trial and non-trial pts were matched 1:1 based on age, sex, number of treatment regimens prior to HMA (for non-trial pts) or experimental regimen (for trial pts) and IPSS-R categories. All non-trial pts included in the analysis received at least 4 cycles of AZA or DAC at the same institution. Transplant rates and overall survival (OS) were evaluated for association with trial participation. OS was estimated by the Kaplan-Meier method and compared using Cox proportional hazard regression with two-sided Wald test with adjustment for matching variables. The relative odds of transplant following initial treatment were estimated using logistic regression and compared with two-sided Wald test.
Results: Of 774 pts in the MDS CRC database for whom complete data were available, 323 were treated in clinical trials and 451 were treated with AZA or DAC. The trial and non-trial MDS cohorts were well matched with regards to median age (68.5 vs 68.2 yrs; P=0.65), females (28.4% vs 29.9%, P=0.75), numbers of regimens (3 vs 3, P=0.77) and IPSS-R risk categories (P=0.86). Estimated median OS of pts treated in and out of clinical trials was 44.5 and 50.6 months (P=0.67), respectively. Compared to standard of care, trial participation was not associated with any survival advantage [Hazard ratio (HR), 95% CI, 0.94 (0.72-1.24), P=0.67] (Figure 1). Clinical trial participation did not significantly increase the odds of proceeding to transplant [Odds Ratio (OR) (95% CI), 1.5 (0.68, 1.61), P = 0.83)]. As shown in Table 1, in multivariate analyses, among all factors, increasing number of regimens received was significantly associated with better survival, possibly reflecting a bias towards healthier pts who survived longer to receive multiple regimens.
Conclusions: In a matched-pair analysis, we found comparable survival outcomes between trial and non-trial higher-risk MDS pts treated at specialty centers. Our matched analysis failed to identify any statistical evidence to suggest that an average patient benefited from trial participation within the MDS CRC sites. Additional research is necessary to interrogate these comparisons for specific patient subpopulations by genetic alterations, co-morbidities and regimen sequence, for which trial participation may have been beneficial. Based on the population-average findings, however, we expect any improvement in survival to be modest.
Komrokji:Celgene: Honoraria, Research Funding; Novartis: Honoraria, Speakers Bureau; Celgene: Honoraria, Research Funding; Novartis: Honoraria, Speakers Bureau; Novartis: Honoraria, Speakers Bureau; Novartis: Honoraria, Speakers Bureau. Roboz:Orsenix: Consultancy; Celltrion: Consultancy; Janssen Pharmaceuticals: Consultancy; Astex Pharmaceuticals: Consultancy; Eisai: Consultancy; Daiichi Sankyo: Consultancy; Novartis: Consultancy; Astex Pharmaceuticals: Consultancy; Celgene Corporation: Consultancy; AbbVie: Consultancy; AbbVie: Consultancy; Eisai: Consultancy; Celltrion: Consultancy; Roche/Genentech: Consultancy; Aphivena Therapeutics: Consultancy; Sandoz: Consultancy; Roche/Genentech: Consultancy; Daiichi Sankyo: Consultancy; Argenx: Consultancy; Jazz Pharmaceuticals: Consultancy; Pfizer: Consultancy; Cellectis: Research Funding; Celgene Corporation: Consultancy; Orsenix: Consultancy; Bayer: Consultancy; Novartis: Consultancy; Bayer: Consultancy; Jazz Pharmaceuticals: Consultancy; Pfizer: Consultancy; Sandoz: Consultancy; Argenx: Consultancy; Otsuka: Consultancy; Aphivena Therapeutics: Consultancy; Janssen Pharmaceuticals: Consultancy; Otsuka: Consultancy; Cellectis: Research Funding. Nazha:MEI: Consultancy. Maciejewski:Apellis Pharmaceuticals: Consultancy; Alexion Pharmaceuticals, Inc.: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Ra Pharmaceuticals, Inc: Consultancy; Apellis Pharmaceuticals: Consultancy; Ra Pharmaceuticals, Inc: Consultancy; Alexion Pharmaceuticals, Inc.: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Sekeres:Celgene: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Opsona: Membership on an entity's Board of Directors or advisory committees; Opsona: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal